The amount of sleep you get every night affects your well-being, but the quality of your sleep makes a difference too. According to the Centers for Disease Control, inadequate sleep doesn’t just make you tired, it can increase the risk of diabetes, cardiovascular disease, stroke, obesity, and depression.
“Not only does insufficient sleep put people at risk for chronic diseases, but it also contributes to motor vehicle crashes and machinery-related injuries,” said Manning Regional Healthcare Center (MRHC) Respiratory Therapist, Tina Gehling, RRT, RCP, BSHM, EMT.
For those struggling to sleep, Gehling offers these tips for a more restful night:
- Stick to a sleep schedule
- Pay attention to what you eat and drink
- Create a restful environment
- Limit daytime naps
- Include physical activity in your daily routine
- Manage stress
- Contact your primary care provider if you continue to struggle sleeping
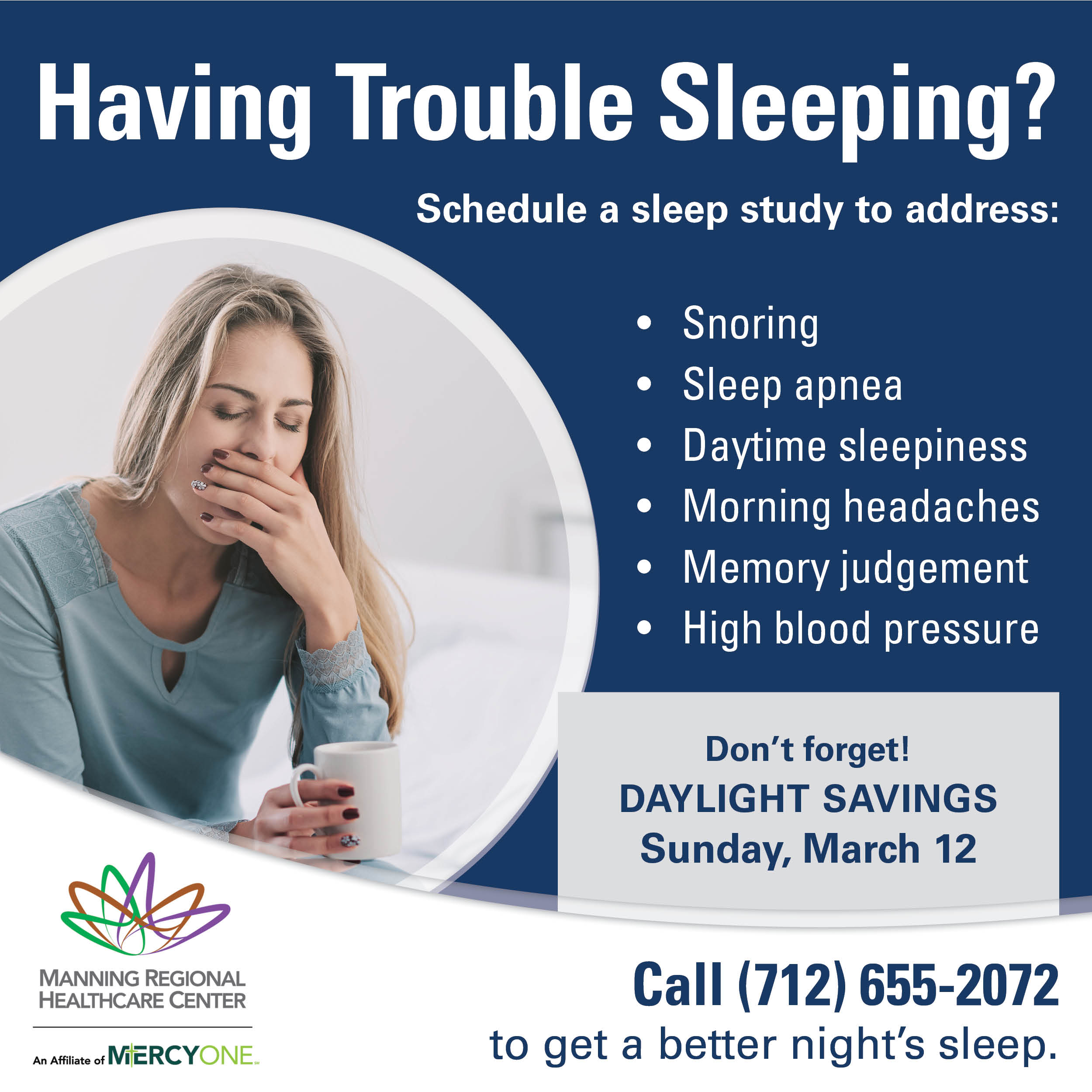
Daylight savings will take effect on March 12 – causing all of us to “lose” an hour of sleep. But if you are among those whose sleep continues to suffer, there may be a reason, other than the time change, to blame.
“Nearly everyone has an occasional sleepless night — but if you often have trouble sleeping, contact your doctor. Identifying and treating any underlying causes can help you get the better sleep you deserve,” said Gehling.
If you are having trouble sleeping, repeatedly waking up in the middle of the night, waking up not feeling rested or experiencing weight gain, obesity, or even snoring, it could be because of your sleeping habits. To diagnose and treat sleep disorders, MRHC recommends completing a sleep study. Testing can be completed in one night in the convenience of the patient’s own home with the ability for the patient to go to work immediately after the study.
“By doing at-home sleep studies, we are able to put patients on an autoPAP if results show they have sleep apnea, a very common disorder,” said Gehling.
Sleep apnea is a potentially life-threatening sleep disorder that staff routinely see. Gehling notes this is a condition in which there is a delay in breathing that can last for at least ten to 30 seconds during sleep. In severe cases, this can happen multiple times a night without the individual noticing or waking up. As a result, sleep apnea has been linked to heart attacks, heart arrhythmias, and strokes. If left untreated, sleep apnea can be deadly.
Some symptoms of sleep apnea include daytime sleepiness or fatigue, morning headaches, frequent nighttime urination, loud snoring, irritability, and more. Risk factors include family history, neck circumference, large tonsils, and age – among many others.
Sleep Apnea Questionnaire
Do you:
Snore or have been told that you snore?
Sleep during the day?
Feel drowsy when driving?
Wake up with morning headaches?
Have frequent memory or judgement problems?
Experience frequent irritability?
Noticed mood changes?
Wake up and/or make frequent trips to the bathroom during the night?
Weigh 20% or more than your ideal body weight?
Have a neck size 17 inches or greater (male) or 16 inches are greater (female)?
Have high blood pressure?
Have a decrease in sexual drive?
If you answered “yes” to any of these questions, consult with your primary care provider about scheduling a sleep study by calling (712) 655-2072.